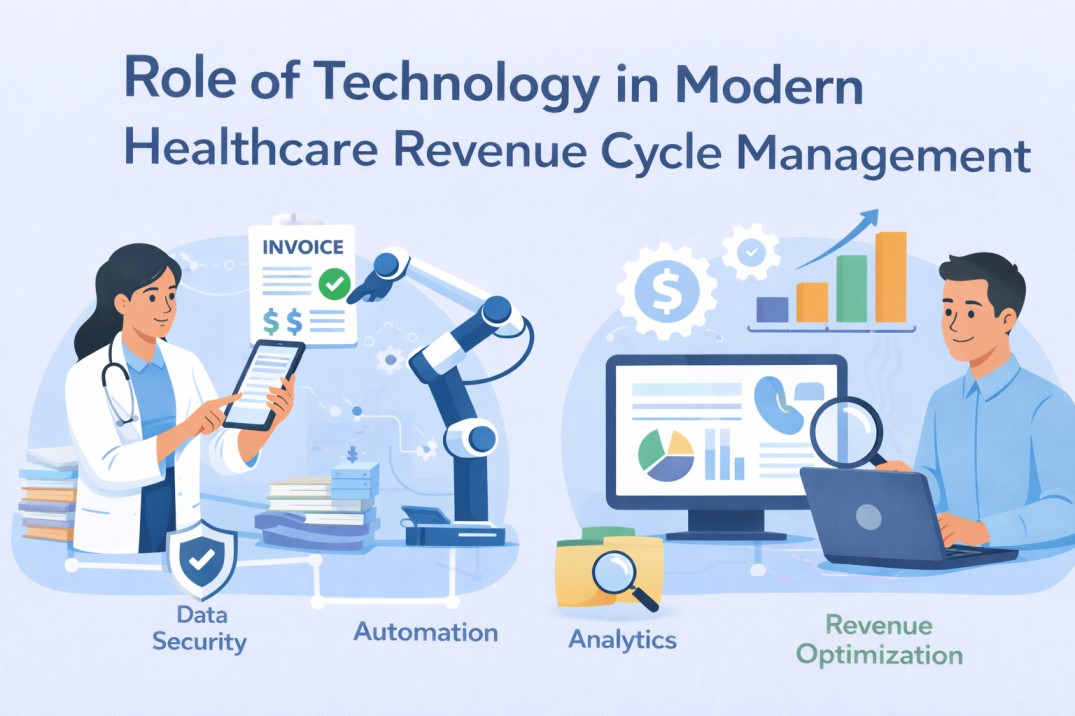
Healthcare organizations today operate in an increasingly complex financial environment. Rising patient responsibility, changing payer regulations, and growing administrative workloads have made it difficult for practices to maintain consistent cash flow. In this landscape, technology has become a critical driver of efficiency and accuracy in healthcare revenue cycle management. From patient registration to final payment posting, modern tools are transforming how providers manage revenue, reduce errors, and improve overall financial performance.
Understanding Revenue Cycle Management in Healthcare
Revenue cycle management refers to the entire financial process that healthcare providers use to track patient care episodes from initial appointment scheduling to final reimbursement. This cycle includes eligibility verification, medical coding, claims submission, payment posting, denial management, and patient collections. Even small inefficiencies in any stage can lead to delayed payments, claim denials, or lost revenue. Technology now plays a central role in closing these gaps and ensuring smoother financial operations.
Automation at the Front End of the Revenue Cycle
The revenue cycle begins before a patient ever receives care. Technology-driven patient registration systems help capture accurate demographic and insurance information at the start, reducing errors that often lead to claim rejections. Automated eligibility verification tools check coverage in real time, allowing staff to identify copays, deductibles, and non-covered services upfront. This not only improves billing accuracy but also enhances transparency for patients and reduces collection challenges later in the cycle.
Technology-Driven Medical Coding Accuracy
Medical coding is one of the most error-prone stages of revenue cycle management. Coding inaccuracies can result in underpayments, audits, or outright denials. Modern coding software uses built-in compliance checks, payer-specific rules, and intelligent prompts to guide coders toward accurate code selection. Advanced systems also integrate directly with electronic health records, reducing manual data entry and ensuring documentation supports billed services. This technological support significantly improves claim accuracy and reimbursement rates.
Streamlining Claims Submission and Processing
Claims submission is no longer a manual or fragmented process. Technology enables automated claim scrubbing that identifies errors before claims are sent to payers. These systems check for missing modifiers, incorrect patient data, and payer-specific requirements, reducing the likelihood of denials. Electronic claims submission platforms also allow practices to submit claims faster and track their status in real time, improving visibility across the revenue cycle.
Enhancing Denial Management Through Data and Analytics
Denials are a major source of revenue loss for healthcare providers. Technology has transformed denial management by providing detailed analytics and reporting tools. These systems identify denial trends, root causes, and payer behaviors, allowing practices to take proactive steps to prevent repeat issues. Instead of reacting to denials after they occur, organizations can use data insights to improve documentation, coding practices, and front-end processes that directly impact claim acceptance.
Improving Payment Posting and Reconciliation
Automated payment posting tools simplify one of the most time-consuming revenue cycle tasks. These systems match payments to claims, post adjustments accurately, and flag underpayments for follow-up. Electronic remittance advice integration reduces manual errors and speeds up reconciliation. As a result, billing teams spend less time on administrative work and more time focusing on revenue optimization strategies.
Technology’s Role in Patient Billing and Collections
Patient billing has become increasingly important as patients shoulder more financial responsibility. Modern billing platforms generate clear, easy-to-understand statements and offer multiple payment options, including online portals and automated payment plans. These tools improve patient engagement and increase the likelihood of timely payments. Transparent billing supported by technology also builds trust and reduces disputes that can delay revenue collection.
Supporting Compliance and Regulatory Requirements
Healthcare billing is governed by strict regulations that continue to evolve. Technology helps practices stay compliant by automatically updating coding rules, payer policies, and regulatory guidelines. Audit trails, secure data storage, and role-based access controls protect sensitive financial information while supporting compliance with healthcare data protection standards. This reduces the risk of penalties, audits, and legal challenges that can negatively impact revenue.
Integrating Systems for a Unified Revenue Cycle
One of the biggest advantages of technology in modern revenue cycle management is system integration. When practice management software, electronic health records, and billing platforms work together seamlessly, data flows smoothly across departments. This integration reduces duplication, improves communication between clinical and billing teams, and creates a more accurate and efficient revenue cycle. A unified system also provides leadership with real-time financial insights to support strategic decision-making.
Preparing for the Future of Revenue Cycle Management
As healthcare continues to evolve, technology will play an even greater role in revenue cycle management. Artificial intelligence, predictive analytics, and machine learning are already being used to forecast cash flow, identify high-risk claims, and optimize staffing resources. Practices that invest in modern technology are better positioned to adapt to industry changes, manage financial challenges, and sustain long-term growth.
Conclusion
Technology has become the backbone of modern healthcare revenue cycle management. By automating routine tasks, improving accuracy, enhancing visibility, and supporting compliance, technology empowers healthcare providers to manage their finances more effectively. Practices that embrace digital tools across the revenue cycle are not only improving operational efficiency but also ensuring financial stability in an increasingly demanding healthcare environment.